Every year, dozens of workers die and thousands more become seriously ill while working in hot or humid conditions — most of these incidents are entirely preventable.
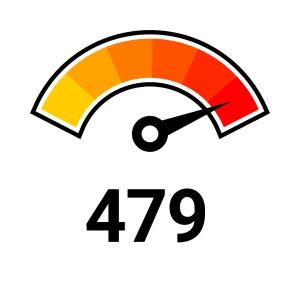

Death and injury and illness figures are likely vast underestimates, due to misreporting or misclassification. Sources: OSHA, National Safety Council.
The human body normally cools itself through sweating, but when exposed to more heat than it can handle, that system can fail. If not addressed, heat exhaustion and heat stroke can escalate quickly, leading to delirium, organ damage, and even death.
While most people recognize the dangers of outdoor heat stress, indoor heat hazards are often overlooked — especially in environments like kitchens, warehouses, or near machinery without proper climate control.
The American Industrial Hygiene Association (AIHA) offers a mobile Heat Stress App to help both outdoor and indoor workers assess heat risk in real time.
Workers have suffered heat-related illnesses across a wide range of industries, both indoors and outdoors. Below are examples of environments where hazardous heat exposure is a concern:
Outdoors
– Agriculture
– Construction (especially road, roofing, and other outdoor work)
– Landscaping
– Mail and package delivery
– Oil and gas well operations
Indoors
– Bakeries, kitchens, and laundries (with heat-generating appliances)
– Electrical utilities (particularly boiler rooms)
– Fire service
– Iron and steel mills and foundries
– Manufacturing with local heat sources, such as furnaces (e.g., paper or concrete production)
– Warehousing
OSHA has made strides to protect workers from heat-related hazards. In July 2024, the agency introduced a Heat Injury and Illness Prevention proposed rule, requiring employers to provide water, shade, rest breaks, training, and heat illness prevention plans for both indoor and outdoor workers. This milestone builds on OSHA’s National Emphasis Program and formalizes protections under enforceable standards.

– New or unacclimated workers
– Older adults
– Pregnant workers
– Individuals with chronic conditions (heart disease, diabetes)
– Workers wearing heavy protective clothing or PPE
– Those working in hot indoor environment (e.g., warehouses, kitchens)
– Heavy physical activity
– Warm or hot environmental conditions
– Lack of acclimatization
– Wearing clothing that traps body heat

Acclimatization is the result of beneficial physiological adaptations — think improved sweating efficiency and stabilized circulation — that develop when workers are gradually exposed to hot conditions. Employers should ensure that all workers are properly acclimatized before they begin work in a hot environment.
Best practices for employers:
Gradually increase workers’ time in hot conditions over 7 to 14 days
For new workers:
– No more than 20% of the usual duration of work in the heat on day 1
– Increase by no more than 20% each additional day
For experienced workers returning to the heat:
– Day 1: No more than 50%
– Day 2: No more than 60%
– Day 3: No more than 80%
– Day 4: Full schedule (100%)
– Closely supervise new employees for the first 14 days or until they are fully acclimatized
– Workers who are not physically fit may need more time
– Acclimatization can be maintained for a few days without heat exposure
– Taking breaks in air conditioning does not reverse acclimatization
> View the National Institute for Occupational Safety and Health (NIOSH) acclimatization fact sheet.
PPE can increase the risk of heat stress because it often restricts airflow and reduces the body’s ability to dissipate heat. Employers must factor this into their heat illness prevention planning.
Strategies to reduce risk when using PPE:
– Use the lightest and most breathable materials when appropriate
– Schedule work requiring PPE during cooler parts of the day
– Rotate employees to reduce prolonged exposure in PPE
– Provide additional hydration and rest breaks for PPE-wearing workers

External Resources
– OSHA Heat Illness Prevention
– Heat.gov
– CDC Heat and Health
– NIOSH Heat Stress Guide
– AIHA Thermal Heat Stress Resources
– NSC Injury Facts: Weather-Related Deaths
– Safety+Health Magazine: Heat Safety Articles
State Resources
While heat can be dangerous anywhere, employers in hotter regions must take extra precautions. If you’re operating in Arizona, Nevada, or New Mexico, check for updated guidance from:
Arizona:
– AZ Department of Health Services
– Maricopa County Extreme Heat Resources
– Industrial Commission of Arizona – Heat Stress Awareness
– Heat Relief Network
Nevada:
– NV OSHA Heat Illness Regulation Announcement
– Heat Illness Prevention Guidance (PDF)
– Clark County Heat Safety
New Mexico:
– NM OSHA: Heat Illness and Injury Prevention
– 2025 Heat Rule Fact Sheet for Employers (PDF)
– Pioneering Study Reveals Heat Stress Risks for Construction Workers (University of New Mexico article)
NSC/ACNSC Tools and Resources
Available to Everyone:
– Traditional, Innovative Approaches for Addressing Occupational Heat Stress (NSC Article)
– NSC Position/Policy Statement: Extreme Temperatures (PDF)
– Surviving the Hot Weather (NSC web page)
– NIOSH Heat Stress Guide
Exclusive to Members (accessible when logged in):
– Heat Illness Safety Talk (PDF)
– Beat the Heat Poster (PDF)
– Stay Safe in the Heat Poster (PDF)
– Heat Kills Poster (PDF)
– Hot Weather Safety Tip Sheet (PDF)
– Summer Safety Tip Sheet (PDF)
– Work Safe This Summer Poster (PDF)
ACNSC members get access to the National Safety Council’s full heat safety resource library.